Chronic Pain Red Flag Checker
Quick Decision Checklist
Tick 'Yes' for each item that applies to your situation. If you answer 'Yes' to two or more items, it may be time to seek professional medical help.
Click "Check My Results" to see if you need professional medical attention.
Important Information
Warning: This tool is for informational purposes only and is not a substitute for professional medical advice. If you experience severe or concerning symptoms, contact your healthcare provider immediately.
Note: If you answer "Yes" to two or more questions, it's recommended to consult with your primary care physician or visit an urgent care clinic.
Living with chronic pain can feel like walking a tightrope-one day you’re steady, the next a sudden jolt threatens to throw you off balance. Most of us learn to cope, but there comes a point when the pain stops being manageable and starts demanding urgent attention. This guide helps you spot those tipping points, decide when to call in professional help, and use practical tools while you wait for care.
What Is Chronic Pain?
In the medical world, Chronic Pain is defined as pain lasting longer than three months or beyond the usual healing time of an injury. Unlike acute pain, which serves as a warning sign, chronic pain persists, often without a clear cause, and can reshape daily life. Common sources include arthritis, nerve damage, back disorders, and conditions like fibromyalgia.
Red Flags: When Pain Crosses the Line
Most people develop a personal pain threshold, but certain patterns signal that your body is flagging a serious problem. Look out for these physical and emotional warning signs:
- Sudden increase in intensity that doesn’t respond to usual medication.
- New symptoms such as numbness, weakness, or loss of bladder/bowel control.
- Pain that wakes you up at night or disrupts sleep consistently.
- Persistent fatigue, weight loss, or fever alongside pain.
- Feelings of hopelessness, depression, or anxiety that intensify with the pain.
When more than one of these appears, it’s a clear cue to seek professional evaluation.
Physical Signs That Something’s Wrong
A pain flare-a rapid spike in discomfort-can be a normal part of chronic conditions, but some features suggest it’s more than a flare:
| Symptom | Why It Matters |
|---|---|
| Sharp, localized pain | May indicate tissue damage or nerve compression |
| Progressive weakness | Could signal spinal cord involvement |
| Unexplained fever | Suggests infection or inflammation |
| Changes in skin color or temperature | May be vascular or neurological |
Even if you’re unsure, jot these down in a pain diary. A clear record helps clinicians pinpoint the issue faster.
Emotional and Cognitive Impact
Chronic pain doesn’t stay in the body-it seeps into thoughts and moods. Many patients report a "pain‑depression loop" where lingering discomfort fuels negative thinking, which in turn amplifies the perception of pain. If you notice any of the following, consider them signals to reach out:
- Loss of interest in hobbies you once loved.
- Difficulty concentrating or remembering simple tasks.
- Increased irritability or social withdrawal.
These mental health changes are not optional side effects; they’re part of the chronic pain picture and deserve the same attention as physical symptoms.
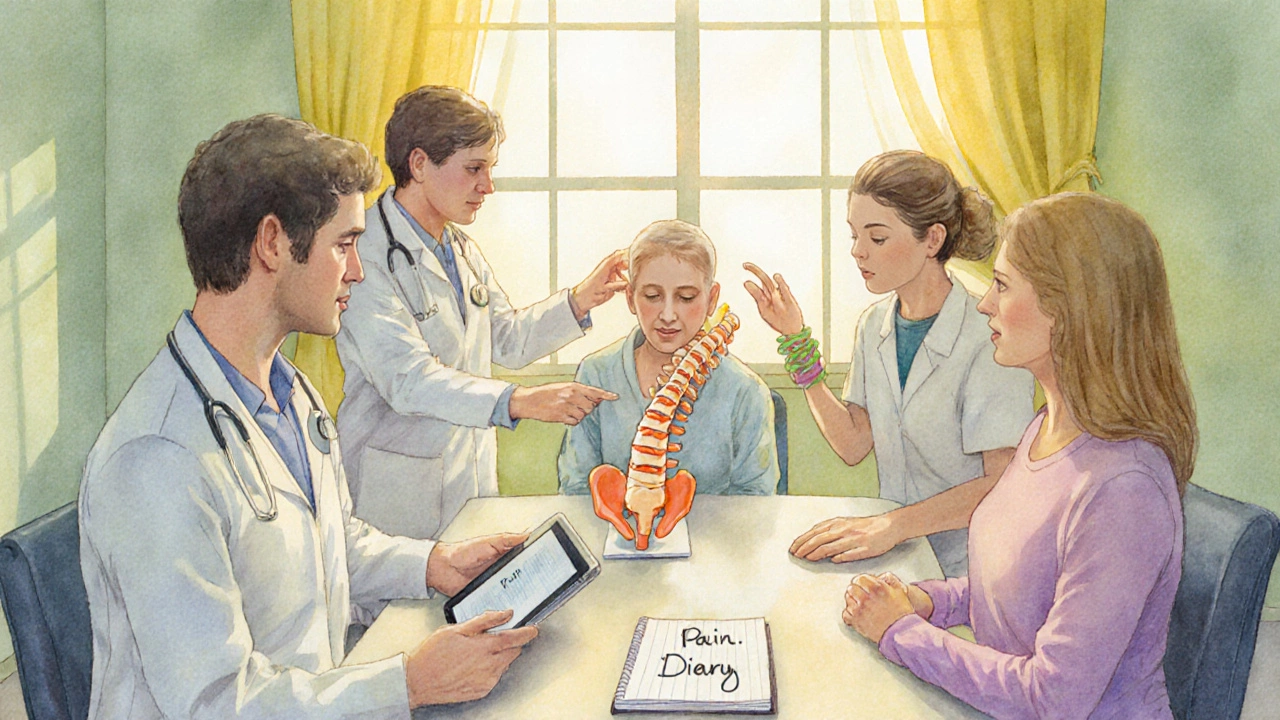
Who Should You Contact?
The first line of defense is usually your Primary Care Physician, who can assess whether the pain signals a new medical issue, adjust medications, or refer you to specialists.
If the pain is complex, a referral to a Pain Specialist-often a anesthesiologist or neurologist with training in pain pathways-can open doors to advanced therapies like nerve blocks or spinal stimulation.
For people whose pain is linked to injuries or musculoskeletal conditions, a Physical Therapist can design movement programs that reduce strain and improve function.
When mood swings, anxiety, or depression dominate the picture, integrating Mental Health Support-counselors, psychologists, or psychiatrists-into the care plan is crucial.
And if opioids have become part of your regimen, discuss any concerns with a clinician well‑versed in Opioid Medication management to avoid dependence and explore safer alternatives.
What to Expect in a Professional Evaluation
During a visit, expect a thorough review that includes:
- Detailed history of pain patterns, triggers, and coping strategies.
- Physical exam focused on neurologic and musculoskeletal function.
- Potential imaging (X‑ray, MRI) if red‑flag signs suggest structural issues.
- Laboratory tests if infection or systemic disease is suspected.
- Discussion of a multidisciplinary Pain Management plan that may combine medication, therapy, and lifestyle changes.
Clinicians often use the WHO analgesic ladder as a guide, starting with non‑opioid options and escalating only when necessary. This stepwise approach helps balance relief with safety.
Self‑Management While You Wait
Even before your appointment, a few low‑risk actions can keep the pain from spiraling:
- Track your pain: Use a notebook or app to log intensity (0‑10 scale), triggers, medication doses, and sleep quality.
- Gentle movement: Short walks, stretching, or yoga can improve circulation and release endorphins.
- Heat or cold therapy: Apply a warm pack for muscle stiffness, a cold pack for inflammation-never exceed 20 minutes per session.
- Mind‑body techniques: Deep breathing, guided meditation, or progressive muscle relaxation can lower stress hormones that heighten pain perception.
- Nutrition check: Anti‑inflammatory foods like fatty fish, leafy greens, and berries may modestly reduce systemic inflammation.
These measures are not substitutes for medical care, but they can buy you time and improve overall wellbeing.
Quick Decision Checklist
| Checklist Item | Yes/No |
|---|---|
| Pain intensity > 7/10 for more than a week | |
| New neurological symptoms (numbness, weakness) | |
| Sleep consistently disrupted by pain | |
| Unexplained fever, weight loss, or swelling | |
| Feeling stuck, hopeless, or increasingly anxious | |
| Current meds no longer effective or cause side effects |
If you tick “Yes” on two or more rows, call your primary care physician or go to an urgent care clinic. Early intervention often prevents chronic pain from becoming a more entrenched condition.
Frequently Asked Questions
How do I differentiate a normal pain flare from a serious red‑flag symptom?
A regular flare usually follows a known pattern and eases with your usual meds or rest. Red‑flag symptoms-like sudden numbness, loss of bladder control, fever, or a sharp pain that wakes you at night-are atypical and warrant prompt medical review.
Can I rely on over‑the‑counter painkillers for chronic pain?
OTC options such as ibuprofen or acetaminophen can help mild to moderate pain, but they often lose effectiveness over time. If you find yourself needing higher doses or using them daily, it’s a sign to speak with a healthcare provider about stronger or alternative treatments.
Is it ever safe to stop an opioid prescription on my own?
Stopping opioids abruptly can cause withdrawal symptoms and increased pain. Always discuss tapering plans with a prescriber who can guide you through a gradual reduction and suggest non‑opioid alternatives.
What role does mental health play in chronic pain management?
Mental health and pain are tightly linked. Depression and anxiety can lower pain thresholds, while persistent pain can worsen mood. Addressing both with therapy, counseling, or medication often leads to better overall outcomes.
When should I consider a multidisciplinary pain clinic?
If your pain remains uncontrolled after trying medication, physical therapy, and basic lifestyle changes, a multidisciplinary clinic-where doctors, physiotherapists, psychologists, and pharmacists collaborate-can offer personalized, integrated care.
Ultimately, chronic pain is a signal, not a sentence. By recognizing the red flags, seeking the right professionals, and using evidence‑based self‑care, you can turn the tide before the pain overwhelms your life.
